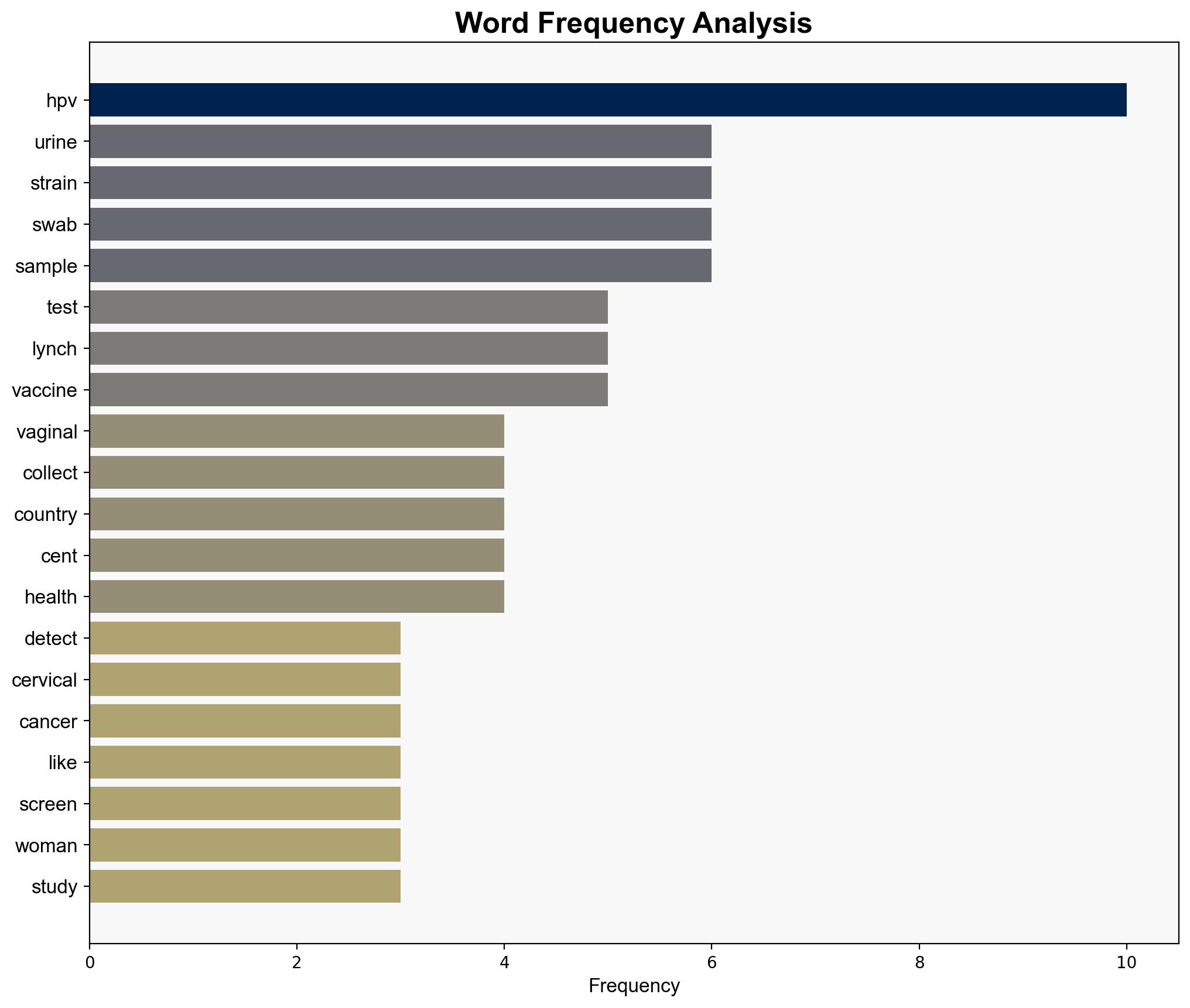
Urine tests detect high-risk HPV as effectively as DIY vaginal swabs – New Scientist
Published on: 2025-08-28
Intelligence Report: Urine tests detect high-risk HPV as effectively as DIY vaginal swabs – New Scientist
1. BLUF (Bottom Line Up Front)
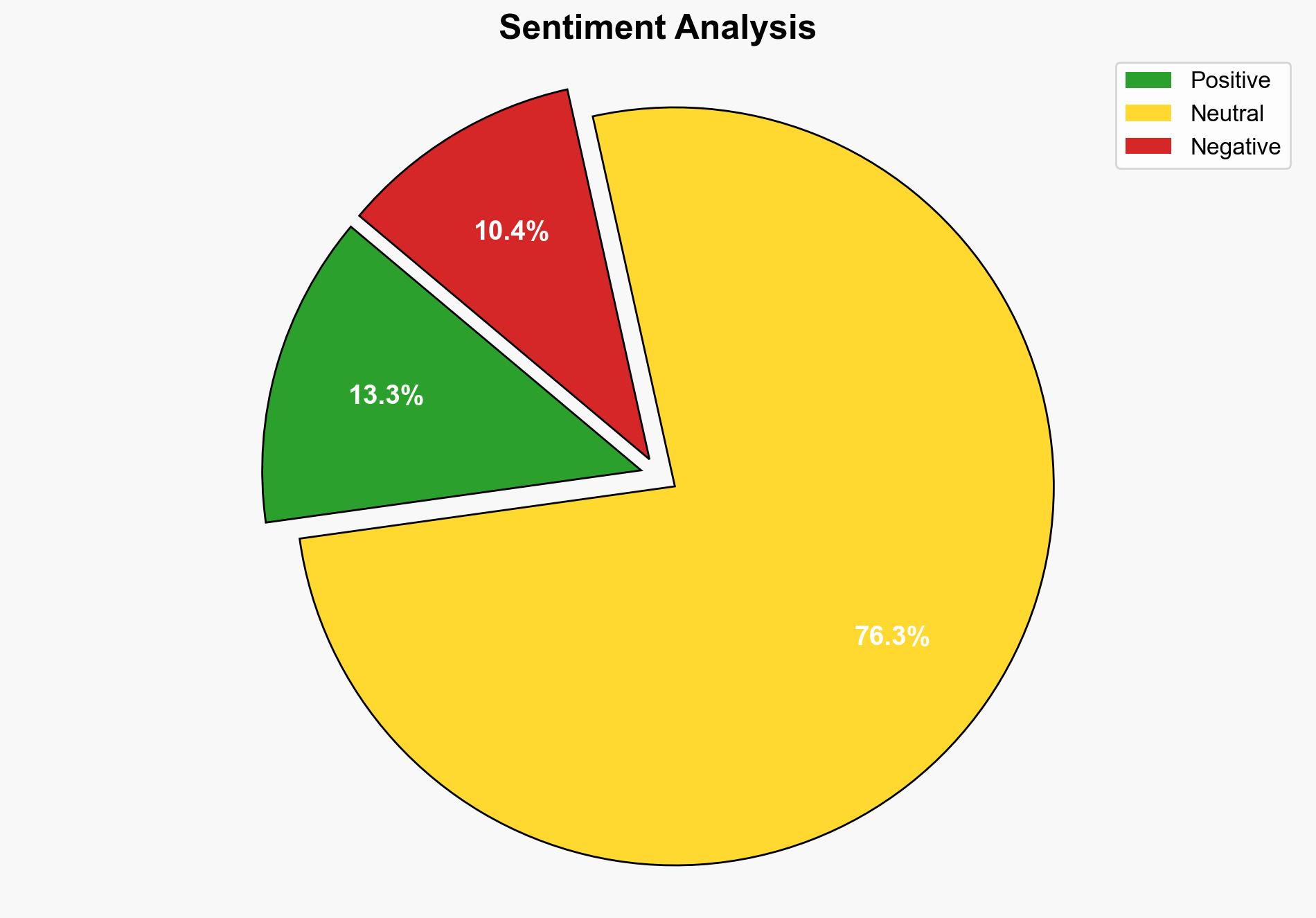
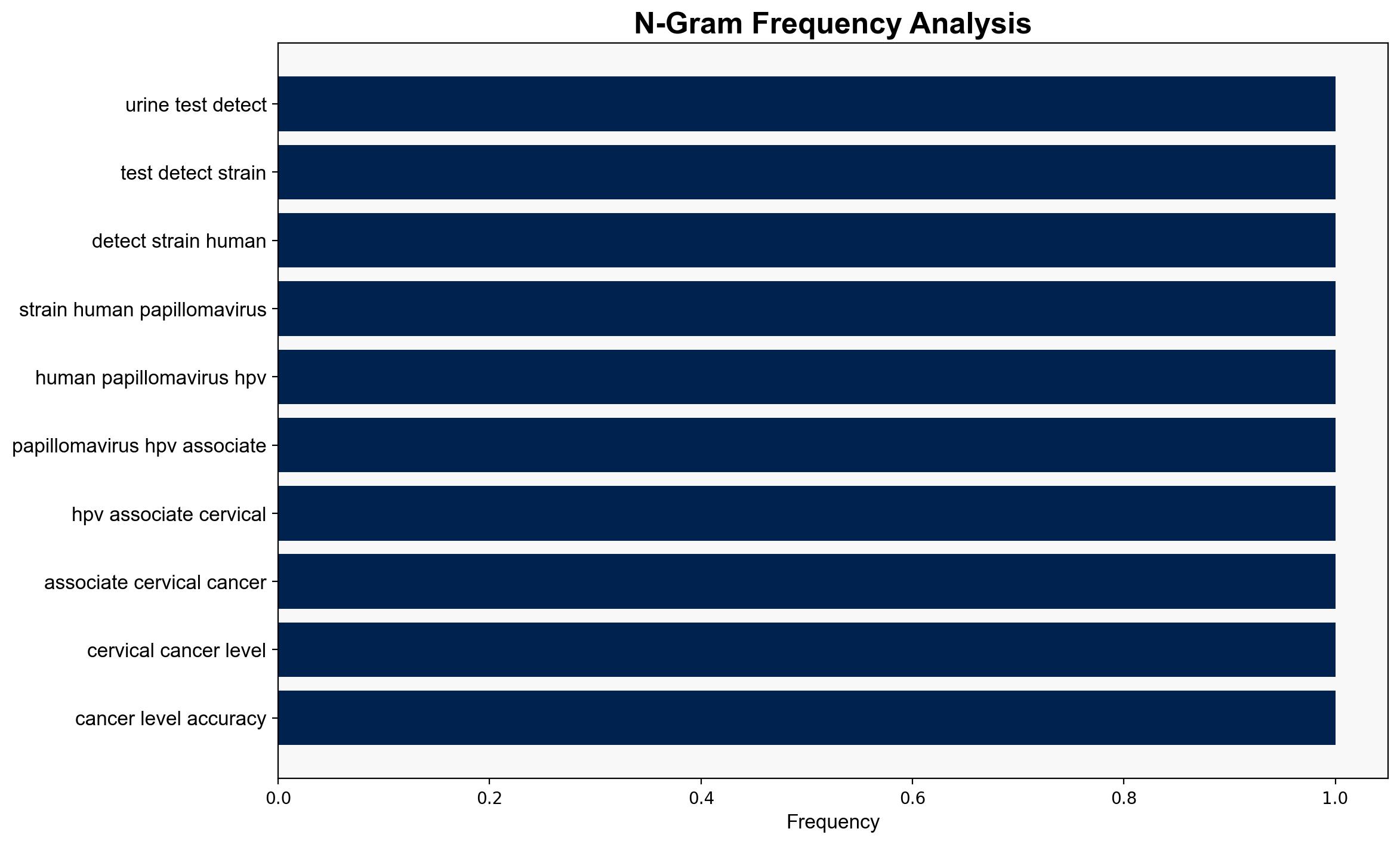
The strategic judgment is that urine tests could potentially revolutionize cervical cancer screening by providing a non-invasive, accessible alternative to traditional methods, particularly in low-resource settings. The hypothesis that urine tests are as effective as DIY vaginal swabs is better supported by the current evidence. Confidence level: Moderate. Recommended action: Encourage further research and pilot programs to validate findings across diverse populations.
2. Competing Hypotheses
1. **Hypothesis A**: Urine tests are as effective as DIY vaginal swabs in detecting high-risk HPV strains, offering a viable alternative for cervical cancer screening.
2. **Hypothesis B**: Urine tests are less effective than DIY vaginal swabs, and their perceived effectiveness is due to limited sample size and geographic scope of the study.
Using ACH 2.0, Hypothesis A is better supported due to the nearly identical detection rates reported in the study, suggesting similar efficacy. However, the limited geographic scope and sample size introduce uncertainty.
3. Key Assumptions and Red Flags
– **Assumptions**: The study assumes that the sample population is representative of broader demographics. It also presumes that the testing conditions in the study can be replicated in real-world settings.
– **Red Flags**: Limited geographic scope (Bangladesh, Pakistan, Nepal) may not reflect global applicability. Potential bias in self-reported data and lack of long-term follow-up data.
– **Blind Spots**: The study does not address potential cultural resistance to urine testing or logistical challenges in implementing widespread urine-based screening.
4. Implications and Strategic Risks
– **Economic**: Adoption of urine tests could reduce healthcare costs by minimizing the need for clinical visits and specialized personnel.
– **Geopolitical**: Countries with limited healthcare infrastructure may benefit, potentially reducing global health disparities.
– **Psychological**: Increased screening uptake due to non-invasive methods could lead to earlier detection and treatment, improving public health outcomes.
– **Risks**: Over-reliance on preliminary findings without broader validation could lead to ineffective screening programs.
5. Recommendations and Outlook
- Conduct larger-scale studies across diverse populations to validate findings and ensure global applicability.
- Develop pilot programs in low-resource settings to assess feasibility and acceptance of urine-based screening.
- Scenario Projections:
- Best Case: Successful validation leads to global adoption, reducing cervical cancer rates significantly.
- Worst Case: Inadequate validation results in ineffective screening, wasting resources and undermining public trust.
- Most Likely: Gradual adoption with phased validation studies, leading to incremental improvements in screening practices.
6. Key Individuals and Entities
– Julia Lynch
– Beverly Green
7. Thematic Tags
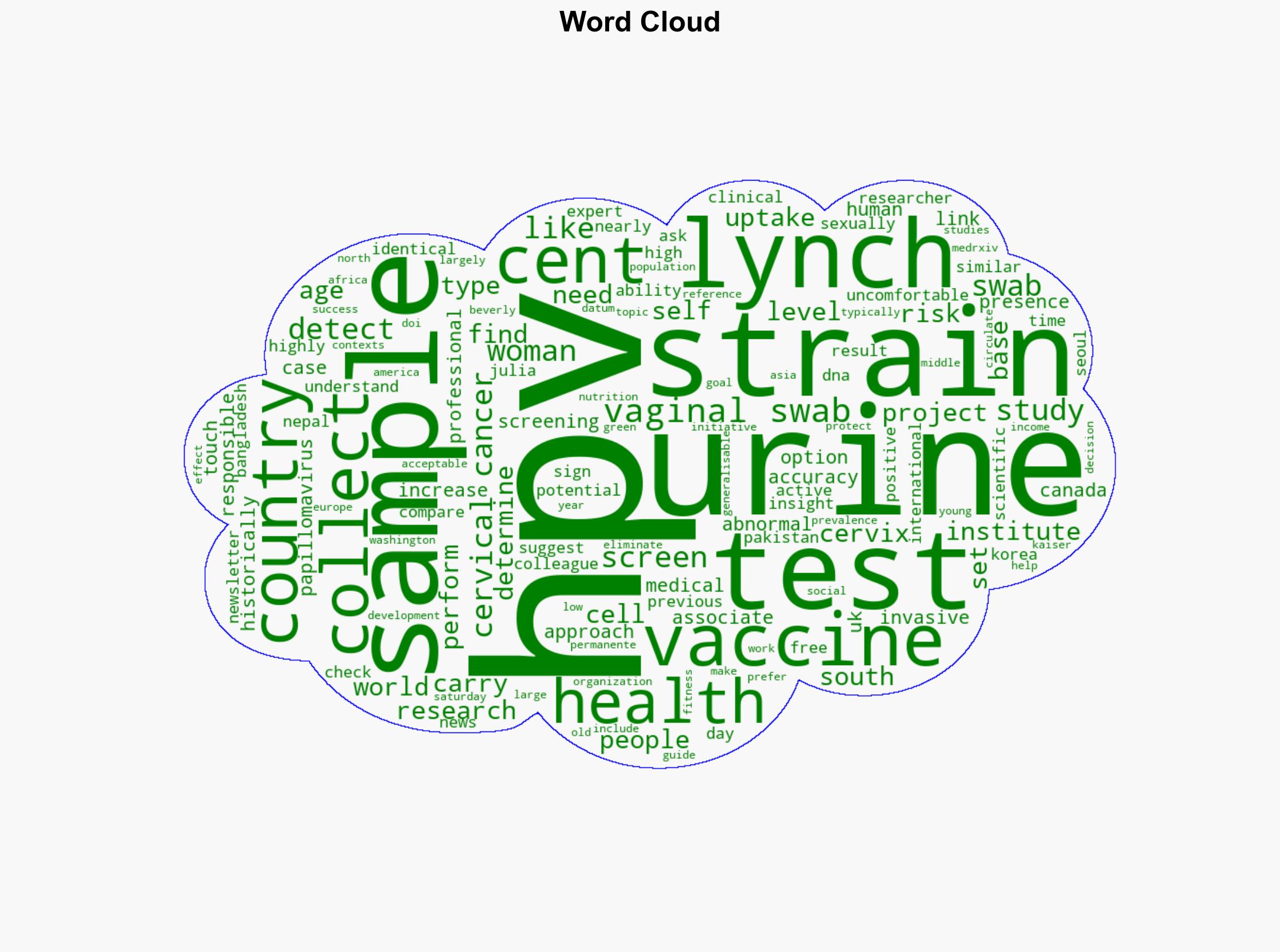
public health innovation, medical technology, global health equity, preventive healthcare